Kedar K. V. Mate, PT PhD1; Brittany R. Lapin, PhD MPH2,3; and David Sugano, DrPH2
1Faculty of Medicine and Health Sciences, McGill University, Montreal, Quebec, Canada
2Department of Quantitative Health Sciences, Lerner Research Institute, Cleveland Clinic, USA
3Neurological Institute Center for Outcomes Research and Evaluation, Cleveland Clinic, USA
Survival of people following catastrophic events or diagnoses has dramatically improved due to advances in medicine. More people are now living with one or more chronic health conditions. A minority of these people find it difficult to adjust to their “new normal” and cannot accommodate their new condition and thus perceive their quality of life (QOL) to be lower. QOL is an increasingly important component of patient-centered care. For patients diagnosed with chronic disabilities, QOL initially declines but typically returns to pre-condition levels due to patients accommodating to their new normal. Others are unable to accommodate and continue to seek services to improve their QOL to little avail. As QOL is determined not only by the patient’s clinical condition but also by how well they adjust, it is critical for patients to actively participate, if not control, this aspect of recovery.
The current healthcare system approach is a deficit-based approach. In other words, it attempts to ‘fix’ what is wrong with an organ or organ system, for instance, achieving a normal value in a laboratory test such as lipid profile. While the deficit-based approach may work early in the course of a disease or where pre-disease health status is a realistic outcome, this approach may be counterproductive in chronic conditions where little or no change in function is possible. Identifying a new phenotype of chronic disability/disease patients who cannot adjust or accommodate to their diminished health state and report poor QOL is an important goal. Currently, the majority of services for chronically ill patients typically go to a minority of patients who are the most dissatisfied with the QOL in their condition. In a fee-for-service system, this drives costs up with little gain in clinical improvement. As QOL researchers within a healthcare system, we propose that care paths focus more on helping patients create a new normal as a critical part of their restorative or rehabilitative service, which will improve their QOL while also potentially reducing unnecessary health costs and improving the satisfaction of both patients and care providers.
The WHO has defined quality of life as individuals’ perception of their position in life in the context of the culture in which they live and in relation to their goals, expectations, standards, and concerns. In the context of health research, QOL goes beyond a description of health status and rather is a reflection of the way that people perceive and react to their health status and to other nonmedical aspects of their lives. According to Aristotle, QOL would be the best kind of life, the happiest life, which is the life of virtue comprising: (i) intellectual or theoretical contemplation, including scientific activity (considered the primary form of happiness); and (ii) practical or moral virtue including courage moderation, generosity, and justice (the secondary form of happiness). In a modern context, this would imply that one needs to contemplate aspects of life engagement and then act in a moral way or, in other words, be both smart and nice. The ‘disability paradox’ posits that physicians believe people with disabilities have worse QOL compared to those without disabilities, and they are unable to imagine good QOL beyond medical interventions. Yet perhaps status quo health care services for people with chronic conditions are no longer feasible and may also give false hope for improvement/change. Physicians should strive to help patients find other sources of meaning and overall happiness in life. We propose a new intervention framework for people living with chronic conditions using patients’ happiness at the heart of care – a care model designed for the patient and by the patient.
The central assumption in our current model of care for people living with chronic conditions is that these patients are unhappy in their current chronic health state, which could be true as chronic health states are associated with some loss of function, limitations in activities, and participation restriction. What if the person is happy in their current state? We propose using a single item on happiness in the current state as a measure of quality of life and use that as an anchor to drive promoting that health state. A self-reported happy person will be able to avoid unnecessary medical care and truly experience a sense of self-acceptance, environmental mastery, well-being, personal growth, and autonomy. Our efforts should be targeted at helping people achieve these aspects of life despite their current health state. Our framework is founded on an amalgamation of a few theoretical approaches: resilience theory, model of meaning perspective transformation in physical rehabilitation, response shift, transformative learning, and others. We need a unified care approach that is patient-centered and driven by the patients.
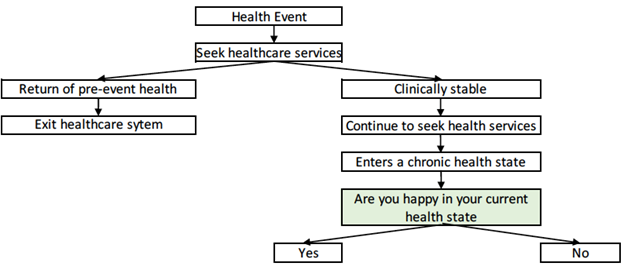
The fact that most patients with disability or chronic illness are ultimately able to enjoy life and do this so well is a testament to the human spirit and ingenuity. As a society and medical community, we should identify and support those patients who cannot make this critical transition and recover their initial QOL. A simple method for identifying these patients is provided in the figure. In this way, we can help these patients maximize their QOL without using limited healthcare services and resources on this unique psychosocial problem.
This newsletter editorial represents the views of the author and does not necessarily reflect the views of ISOQOL.
How to Submit a Newsletter Editorial
Do you have something to share about health related quality of life and patient-centered outcomes? We want to hear from you!
Learn More

The International Society for Quality of Life Research (ISOQOL) is a global community of researchers, clinicians, health care professionals, industry professionals, consultants, and patient research partners advancing health related quality of life research (HRQL).
Together, we are creating a future in which patient perspective is integral to health research, care and policy.
